Nutritional Status and Perceived Stress of Healthcare Professionals in Ekiti State, Nigeria
Abstract
Background: The healthcare profession has been associated with stress which has been found to affect nutritional status.
Purpose: This study was aimed at evaluating the perceived stress-nutritional status nexus of healthcare professionals in Ekiti State, Nigeria.
Methods: This descriptive cross-sectional study involved 414 healthcare professionals. The study sample was obtained by using a two-stage cluster sampling approach. Data on socio-demographic and meal pattern was collected through a pretested self-administered questionnaire.
Results: Body Mass Index (BMI) was obtained from height and weight measurements and classified as underweight (BMI<18.5), normal weight (BMI=18.5-24.99), overweight (BMI=25.0-29.99), obesity (BMI≥30). Perceived stress was evaluated using the perceived stress scale version 10 (PSS-10). Data were analyzed using Statistical package for social sciences (SPSS) version 26 and subjected to Chi-square test and logistic regression analysis to establish relationship and predictors of perceived stress at 5% level of significance. The healthcare professionals’ age was 35.91±9.31 years with 86.2% being ≤ 45 years and 60% were females. Two meals a day were taken by 85.7%. BMI showed 49.3% to be overweight/obese. The mean perceived stress score was 15.02 with 47.6% having high perceived stress. Age (p=0.016), gender (p=0.001), marital status (p=0.001) and professional group (p=0.048) had significant relationship with perceived stress. The association between BMI and perceived stress was not significant (Chi-square = 0.562; p=0.905). Predictors of stress were gender (OR: 0.505, CI=0.308-0.830; p=0.007) and marital status (OR: 1.914, CI=1.143-3.208; p=0.014).
Conclusion: The study showed high level of obesity and perceived stress. Nutrition education intervention is recommended.
-
Page Number : 1-12
-
Published Date : 2023-10-06
-
Keywords
Stress, Overweight, Obesity, Healthcare professionals -
DOI Number
10.15415/jmrh.2023.101001 -
Authors
O. M. Adeojo, I.O. Dada and K. Ajayi
References
- Adeloye, D., Ige-Elegbede, J., Ezejimofor, M., Owolabi, E., Ezeigwe, N., Omoyele, C., Mpazanje, R., Dewan, M., Agogo, E., Gadanya, M., Alemu, W., Harhay, M., Auta, A., & Adebiyi, A. (2021). Estimating the prevalence of overweight and obesity in Nigeria in 2020: a systematic review and meta-analysis. Annals of Medicine, 53(1), 495–507. https://doi.org/10.1080/07853890.2021.1897665
- Adeolu, J. O., Yussuf, O. B., & Popoola, O. A. (2016). Prevalence and Correlates of Job Stress among Junior Doctors in the University College Hospital, Ibadan. Annals of Ibadan Postgraduate Medicine, 14(2), 92–98.
- Adeomi, A. A., Akande, R. O., Obiajunwa, C., Oduntan, O., & Ogbukwo, E. (2020). Cardiometabolic risk and its association with dietary diversity, activity patterns and the nutritional status of workers in tertiary educational institutions in Southwestern Nigeria. Cardiometabolic Risk and Its Association with Dietary Diversity, Activity Patterns and the Nutritional Status of Workers in Tertiary Educational Institutions in Southwestern Nigeria. Published. https://doi.org/10.21203/rs.3.rs-25987/v1
- Akinsulore, A., Adegbenro, C. A., Balogun, Y. A., Elekwachi, G., Babalola, O. O., & Akinlua, F. M. (2020). Perceived Stress and its Relationship with Coping Strategies among Doctors at a Tertiary Hospital in Ile-Ife, Nigeria. West African Journal of Medicine, 37 (2), 145–151.
- Alao, A. O., Obimakinde, A. M., & Ogunbode, A. M. (2020). Effect of workplace stress on the perceived health of resident doctors in Nigeria. Annals of Ibadan Postgraduate Medicine, 20 (1), 18-25
- Alhassan, R. K., Poku, K. A. (2018). Experiences of frontline nursing staff on workplace safety and occupational health hazards in two psychiatric hospitals in Ghana. BMC Public Health, 18, 701. https://doi.org/10.1186/s12889-018-5620-5
- Alosaimi, F. D., Kazim, S. N., Almufleh, A. S., Aladwani, B. S., & Alsubaie, A. S. (2015). Prevalence of stress and its determinants among residents in Saudi Arabia. Saudi Medical Journal, 36(5), 605–612. https://doi.org/10.15537/smj.2015.5.10814
- Alqarni, T., Alghamdi, A., Alzahrani, A., Abumelha, K., Alqurashi, Z., & Alsaleh, A. (2022). Prevalence of stress, burnout, and job satisfaction among mental healthcare professionals in Jeddah, Saudi Arabia. PLoS ONE, 17(4), e0267578. https://doi.org/10.1371journal.pone. 0267578
- Anwer, S., Manzar, M. D., Alghadir, A. H., Salahuddin, M., & Abdul Hameed, U. (2020). Psychometric Analysis of the Perceived Stress Scale among Healthy University Students. Neuropsychiatric Disease and Treatment, 16, 2389–2396. https://doi.org/10.2147/ndt.s268582
- Asani, M., Farouk, Z., & Gambo, S. (2016). Prevalence of perceived stress among clinical students of Bayero University Medical School. Nigerian Journal of Basic and Clinical Sciences, 13(1), 55. https://doi.org/10.4103/0331-8540.176209
- Banwat, M. E., Haruna, S. A., Vongdip, N. G., Duru, A. K., & Afolaranmi, T. O. (2018). Assessment of the nutritional knowledge, eating habits and nutritional statuses of healthcare workers in Jos, North-Central Nigeria. Research Journal of Food Science and Nutrition, 3(2), 15-22.
- Barrington, W. E., Ceballos, R. M., Bishop, S. K., McGregor, B. A., Beresford, S. A. A. (2012). Perceived Stress, Behavior, and Body Mass Index among Adults Participating in a Worksite Obesity Prevention Program, Seattle, 2005–2007. Prev. Chronic Dis. 9:120001. DOI: http://dx.doi.org/10.5888/pcd9.120001
- Bastianon, C. D., Klein, E. M., Tibubos, A. N., Brähler, E., Beutel, M. E., & Petrowski, K. (2020). Perceived Stress Scale (PSS-10) psychometric properties in migrants and native Germans. BMC Psychiatry, 20(1). https://doi.org/10.1186/s12888-020-02851-2
- Bhelkar, S., Deshpande, S., Mankar, S., & Hiwarkar, P.(2018). Association between stress and hypertension among adults more than 30 Years: A case-control study. National Journal of Community Medicine ,9(6) , 430-433.
- Birhanu, M., Gebrekidan, B., Tesefa, G., & Tareke, M. (2018). Workload determines workplace stress among health professionals working in Felege-Hiwot referral Hospital, Bahir Dar, Northwest Ethiopia. Journal of Environmental and Public Health, 1–8. https://doi.org/10.1155/2018/6286010
- Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A Global Measure of Perceived Stress. Journal of Health and Social Behavior, 24 (4), 385-396.
- Dada, I. (2017). The meal pattern and incidence of overweight and obesity among market women in a Southwest community, Nigeria. Saudi Journal of Obesity, 5(2), 70. https://doi.org/10.4103/sjo.sjo_14_17
- Dada, I., Ajayi, K., & Werimegbe, M. (2021). Exploring mass media to improve fruit consumption pattern of a section of Nigerian adult population. Annals of the Romania Society for Cell Biology, 4604–4616.
- Emond, M., ten Eycke, K., Kosmerly, S., Robinson, L., Stillar, A., & van Blyderveen, S. (2016). The effect of academic stress and attachment stress on stress-eaters and stress-undereaters. Appetite, 100, 210–215. https://doi.org/10.1016/j.appet.2016.01.035
- Gifkins, J., Johnston, A., & Loudoun, R. (2018). The impact of shift work on eating patterns and self-care strategies utilised by experienced and inexperienced nurses. Chronobiology International, 35(6), 811–820. https://doi.org/10.1080/07420528.2018.1466790
- Godifay, G., Worku, W., Kebede, G., Tafese, A., & Gondar, E. (2018). Work related stress among health care workers in Mekelle City administration public hospitals, North Ethiopia. Journal of Health, Medicine and Nursing, 46
- Haile, K. (2017). Assessment of occupational stress and associated factors among nurses in East Gojjam zone public hospitals Northwest Ethiopia. Clinical Medicine Research, 6(2), 43. https://doi.org/10.11648/j.cmr.20170602.13
- Hasen, A. A., Seid, A. A., & Mohammed, A. A. (2023). Anxiety and stress among healthcare professionals during COVID-19 in Ethiopia: systematic review and meta-analysis. BMJ Open 2023, 13: e070367. doi:10.1136/bmjopen-2022-070367
- Hassard, J., Teoh, K. R. H., Visockaite, G., Dewe, P., & Cox, T. (2017). The Cost of Work-Related Stress to Society: A Systematic Review. Journal of Occupational Health Psychology, 23(1), https://www.researchgate.net/publication/313480340 [accessed Dec 03 2021].
- Health and Safety Executive. (2011). Management standards on work-related stress, retrieved from www.hse.gov.uk/stress on 21st August, 2015.
- Hemiö, K., Lindström, J., Peltonen, M., Härmä, M., Viitasalo, K., & Puttonen, S. (2020). The association of work stress and night work with nutrient intake – a prospective cohort study. Scand. J. Work Environ. Health, 46(5), 533–541.
- Honor, W. (2017). Chronic stress may raise obesity risk, Medical news today 2017. https://www.medicalnews today.com
- Huang, F., Wang, H., Wang, Z., Zhang, J., Du, W., Su, C., Jia, X., Ouyang, Y., Wang, Y., Li, L., Jiang, H., & Zhang, B. (2020). Psychometric properties of the perceived stress scale in a community sample of Chinese. BMC Psychiatry, 20(1), https://doi.org/10.1186/s12888-020-02520-4
- Ikujenlola, A., & Adekoya, T. (2020). Nutritional status and feeding habits of females in public and private Universities in Osun State, Southwestern, Nigeria. Heliyon, 6(9), e05023. https://doi.org/10.1016/j.heliyon.2020.e05023
- Isfahani, P., Arefy, M., Peyravi, S., Bahador, R. C., & Afshari, M. (2020). A systematic review and meta-analysis of Job stress among Iranian nurses. A Systematic Review and Meta-Analysis of Job Stress among Iranian Nurses, https://doi.org/10.21203/rs.2.24414/v1
- Joaquim, A., Custódio, S., Savva-Bordalo, J., Chacim, S., Carvalhais, I., Lombo, L., Lopes, H., Araújo, A., & Gomes, R. (2017). Burnout and occupational stress in the medical residents of Oncology, Haematology and Radiotherapy: a prevalence and predictors study in Portugal. Psychology, Health & Medicine, 23(3), 317–324. https://doi.org/10.1080/13548506.2017.1344256
- Kakemam, E., Raeissi, P., Raoofi, S., Soltani, A., Sokhanvar, M., Visentin, C., & Cleary, M. (2019). Occupational stress and associated risk factors among nurses: a cross-sectional study. Contemporary Nurse, 55(2–3), 237–249. https://doi.org/10.1080/10376178.2019.1647791
- Lee, G., Han, K., & Kim, H. (2017). Risk of mental health problems in adolescents skipping meals: The Korean National Health and Nutrition Examination Survey 2010 to 2012. Nursing Outlook, 65(4), 411–419. https://doi.org/10.1016/j.outlook.2017.01.007
- Mucci, N., Giorgi, G., de Pasquale Ceratti, S., Fiz-Pérez, J., Mucci, F., & Arcangeli, G. (2016). Anxiety, stress-related factors, and blood pressure in young adults. Frontiers in Psychology, 7, https://doi.org/10.3389/fpsyg.2016.01682
- Ndejjo, R., Musinguzi, G., Yu, X., Buregyeya, E., Musoke, D., Wang, S., Halage, A., Whalen, C., Bazeyo, W., Williams, P., & Ssempebwa, J. (2015). Occupational health hazards among healthcare workers in Kampala, Uganda. Journal of Environmental and Public Health, https://doi.org/10.1155/2015/913741
- Nemera, A. (2018). Assessment of job related stress and its predictors among nurses working in Government hospitals of West Shoa Zone, Oromia Region, Ethiopia, 2018.
- Nwankwo, C., Karanja, S., & Vasanthakaalam, H. (2017). The occurrence of occupational health hazards in districts health facilities in Kigali, Rwanda. International Journal of Community Medicine And Public Health, 5(1), 21-29. doi:http://dx.doi.org/10.18203/2394-6040.ijcmph20175509
- Odonkor, S. T., & Adams, S. (2021). Predictors of stress and associated factors among healthcare workers in Western Ghana. Heliyon, 7, e07223. https://doi.org/10.1016/j.heliyon.2021.e07223
- Ogba, A. (2020). Occupational stress and its management among health care workers in the University of Port Harcourt Teaching Hospital, Rivers State. Health Science Journal, 14(5), 738.
- Oke, O., & Asamu, F. (2013). Employee perspectives of workplace health promotion in selected institutions in Nigeria. Journal of Research in National Development, 11, 67-74.
- Okwor, T. J., Ndu, A. C., Arinze-Onyia, S. U., Ogugua, I. J., Obionu, I. M., Agwu-Umahi, O. R., Okeke, T. A., & Aguwa, E. N. (2020). Prevalence and Predictors of Stress among Bankers in Enugu State South-East Nigeria. Journal of Community Medicine and Primary Health Care, 32 (2), 68-79. https://dx.doi.org/10.4314/jcmphc.v32i2.6
- Olaitan, O. O., Olanrewaju, O. I., Akinmoladun, F. O., & Fadupin, G. T. (2020). Central Obesity and Stress-Predisposing Factors to Hypertension among Health Workers in Jos University Teaching Hospital, Plateau State, Nigeria. Current Research in Diabetes and Obesity Journal, 12(4), 00111-00116.
- Onigbogi, B., & Banerjee, S. (2019). Prevalence of psychosocial stress and its risk factors among health-care workers in Nigeria: A Systematic Review and Meta-Analysis. Nigerian Medical Journal: Journal of the Nigeria Medical Association, 60 (5), 238–244. https://doi.org/10.4103/nmj.NMJ_67_19
- Ossai, E. N., Alo, A. T., Onwe, B. C., Okoro, D. O., Ezeagu, N. E., & Ogbonnaya, L. U. (2019). Prevalence and Predictors of Perceived Stress: A Study among Medical Students of Ebonyi State University Abakaliki, Nigeria. Asian Journal of Advanced Research and Reports, 1–9. https://doi.org/10.9734/ajarr/2019/v3i129779
- Papier, K., Ahmed, F., Lee, P., & Wiseman, J. (2015). Stress and dietary behaviour among first-year university students in Australia: Sex differences. Nutrition, 31(2), 324–330. https://doi.org/10.1016/j.nut.2014.08.004
- Salilih, Z., & Abajobir, A. (2014). Work-related stress and associated factors among nurses working in public hospitals of Addis Ababa, Ethiopia: A Cross-Sectional Study. Workplace Health & Safety, 62(8), 326–332. https://doi.org/10.1177/216507991406200803
- Sathiya, N., Ruwaidha, R., Nusrath, F., Fathima, F., Gomathy, T., & Shailendra, H. (2016). Perceived stress levels and its sources among doctors and nurses working in a tertiary care teaching hospital, Kancheepuram, Tamil Nadu. International Journal of Community Medicine, 7(7), 603-608.
- Telama, R., Yang, X., Leskinen, E., Kankaanpää, A., Hirvensalo, M., Tammelin, T., Viikari, J. S., & Raitakari, O. T. (2014). Tracking of physical activity from early childhood through youth into adulthood. Medicine and Science in Sports and Exercise, 46(5), 955–962. https://doi.org/10.1249/MSS.0000000000000181
- Uemura, M., Yatsuya, H., Hilawe, E. H., Li, Y., Wang, C., Chiang, C., Otsuka, R., Toyoshima, H., Tamakoshi, K., & Aoyama, A. (2015). Breakfast Skipping is Positively Associated With Incidence of Type 2 Diabetes Mellitus: Evidence From the Aichi Workers’ Cohort Study. Journal of Epidemiology, 25(5), 351–358. https://doi.org/10.2188/jea.je20140109
- Worku, B., Ejigu, Y., & Siraneh, Y. (2020). Occupational Stress and Associated Factors among Nurses working in Public Hospitals of Arsi Zone, Oromia Regional State, Central Ethiopia, 2018. International Journal of Biomedical Engineering and Clinical Science, 6(2), 17. https://doi.org/10.11648/j.ijbecs.20200602.11
- Yubonpunt, P., Kunno, J., Supawattanabodee, B., Sumanasrethakul, C., & Wiriyasirivaj, B. (2022). Prevalence of perceived stress and coping strategies among healthcare workers during the COVID -19 outbreak at Bangkok metropolitan, Thailand. PLoS ONE, 17(7), e0270924. https://doi.org/10.1371/journal.pone.0270924
Introduction:
The healthcare profession has been associated with stress globally (Onigbogi & Banerjee, 2019). According to the American Institute of Stress, 83% of workers in the United States suffered from work-related stress and this accounted for the mortality of 120,000 workers in 2019. In Thailand, the prevalence of stress among healthcare workers was 42% (Yubonpunt et al, 2022). This value is lower compare to 56% prevalence in Saudi Arabia (Alqarni et al, 2022). Previous studies in Ethiopia revealed that 37.8% to 68.2% of healthcare professionals had occupational stress (Salilih & Abajobir, 2014; Birhanu et al., 2018). In 2023, the prevalence of stress in Ethiopia remained high with 51% (Hasan et al, 2023). In Ghana, the prevalence was higher with 70% (Odonkor et al, 2021). In Nigeria, the stress level among the healthcare professionals is also high. In Ile-Ife, a prevalence of 43.2% perceived stress was observed among doctors (Akinsulore et al., 2020). Onigbogi and Banerjee (2019) reported a prevalence of 61.9% of psychosocial stress among healthcare workers in Nigeria. This high prevalence of stress in Nigeria was confirmed by recent studies with 47% in Enugu State (Okwor, 2020) and 62% in Oyo State (Alao et al, 2023). These show higher prevalence rate compared to other developing countries such as Rwanda (15.3%) (Nwankwo et al., 2017), Ghana (17%) (Alhassan & Poku, 2018) and Uganda (21.5%) (Ndejjo et al., 2015). The differences in the degrees of psychosocial stress could be attributed to the structures and administrations of hospitals obtained in the different countries mentioned. An association between work stress and grave economic losses and sub-optimal productivity has been established. This is evidence in the global total estimated cost of work-related stress which ranged from US$221 million to $187 billion annually (Hassard et al., 2017). An estimated cost of £6.7 billion was lost every year by UK industry and 10.8million working days by workers due to work-related stress in 2010/11 (Health & Safety Executive, 2011). These losses emphasize the adverse economic effects of stress.
Stress affects eating behavior in a bidirectional way; it may decrease food intake leading to lose of weight during or after stress. It affects food intake and increases the risk of obesity (Telama et al., 2014). There could be stress-induced overeating and under-eating lifestyles (Emond et al., 2016). Also, meal skipping has been linked with stress (Lee et al.,2017). Papier et al (2015) demonstrated that stress was associated with selection of less healthy foods in individuals. Short term stress can lead to anorexia while long term stress often stimulates intake of comfort food that are high in fat and carbohydrates, and less consumption of fruits which causes high incidence of non-communicable diseases (Honor, 2017; Dada et al., 2021). Stress can stimulate individuals to crave for sugary foods and skip breakfast which can affect their nutritional status (Akinsulore et al., 2020). Work stress brings about reduction in diet quality with increased fat consumption and decreased intakes of micronutrient-rich foods such as fruits and vegetables (Hemio et al., 2020). According to Uemura et al. (2015), skipping of breakfast was found to be positively associated with occurrence of Type 2 diabetes mellitus regardless of their other lifestyles and baseline Body Mass Index. It was also associated with incidence of other cardiovascular diseases.
Furthermore, stress encourages people to use coffee or other stimulants in order to cope. Caffeine stimulates production of increased amount of adrenaline and cortisol hormones which gives an individual under stress to crave for foods that are high in carbohydrates, sugars, and fats. Such eating habits will lead to accumulation of excess fat in the body. Stress produces inadequate consumption of foods and intakes of nutrients which leads to fluctuations in the blood sugar and other metabolic reactions. These fluctuations, coupled with abnormal activation of the sympathetic nervous system triggered by stress lead to problems such as tiredness, lapses of concentration, and mood swings; and cumulates into hypertension, diabetes, obesity (Mucci et al, 2016; Bhelkar et al, 2018). In Nigeria, there is a high prevalence of overweight and obesity with estimated values of 21 million and 12 million respectively in the population aged 15 years or more in 2020 (Adeloye et al., 2021). The health of the healthcare workers is very crucial to the effective discharge of their duties and responsibilities and the way they function at work. (Oke & Asamu, 2013). Increasing work load in many hospitals has been attributed to certain factors which include increasing prevalence of non-communicable diseases (NCDs), the re-emergence of Lassa Fever, the novel coronavirus pandemic, progressive decrease in number of specialist manpower, poor allocation of resources to the health-sector, and medical brain-drain; hence, many healthcare workers skip meal at work (Gifkins et al., 2018), notwithstanding working long hours. This inadequate feeding habits can have adverse effect on their effectiveness at work and make them prone to infections. Few studies have also been carried out on the issue of stress in relation to nutrition in Nigeria. Hence, this study intends to assess the perceived stress of healthcare professionals in relation to their nutritional status in Ekiti State, Nigeria.
1.1 A conceptual framework for perceived stress and nutritional status:
An hypothetical framework for stress and an indicator of poor nutritional status, which is obesity is given below:
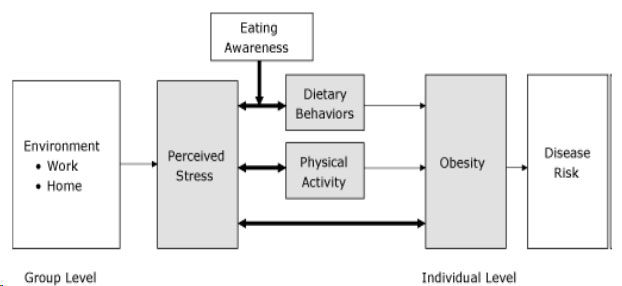 Figure 1: An hypothetical conceptual framework of bio-behavioral relationship between perceived stress and obesity (Barrington et al, 2012)
Figure 1: An hypothetical conceptual framework of bio-behavioral relationship between perceived stress and obesity (Barrington et al, 2012)
The framework shown in figure 1 above associates perceived stress with dietary behaviors and physical activity. It also depicts the link between perceived stress and obesity. At the group level, environmental factors at work and home can contribute to perceived stress which in turn affects dietary behaviors and physical activity leading to obesity. And at the individual level, obesity, which is an indicator of poor nutritional status can lead to disease risk.
Materials and Methods:
2.1 Study design:
This study was descriptive and cross-sectional. It involved healthcare professionals working in tertiary health facilities in Ekiti State, South-Western Nigeria.
2.2 Study area:
Ekiti State is one of the six States in the South-Western part of Nigeria with its capital in Ado-Ekiti. There are two (2) tertiary health care Institutions in Ado-Ekiti, namely- Ekiti State University Teaching Hospital owned by Ekiti State Government and Afe Babalola Multisystem Hospital (privately-owned). The third tertiary health Institution (The Federal Teaching Hospital) is located in Ido-Ekiti and owned by the Federal Government of Nigeria.
2.3 Study population:
The study population was the three selected subgroups of health care professionals (medical doctors, nurses and medical laboratory scientists) in the three tertiary health Institutions in Ekiti State who were presumed to be more exposed to stressful work schedule.
2.4 Inclusion and exclusion criteria:
the participants were the Medical doctors, Medical laboratory scientists and Nurses working in the selected tertiary health care Institutions. However, health care professionals who were on outside posting not located in Ekiti State, those who were retired or who were not actively practicing and health care professionals who were on leave during the time of study were excluded.
2.5 Sample size determination:
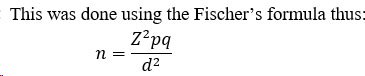
n = the minimum sample size for a population above 10,000
Z = 95% confidence level = 1.96
P = prevalence of perceived stress among medical doctors which was 43.2% (0.432) (Akinsulore et al., 2020)
q = 1- p
d = degree of accuracy desired = 0.05
Therefore,
376.8 + 37.7 = 414
Hence, the minimum sample size used was 414.
2.6 Sampling Technique:
A two-stage cluster sampling technique was used in establishing the study sample. In stage I, a list of all the healthcare professional groups in Ekiti State was obtained and three (3) professional groups (doctors, nurses and medical laboratory scientists) were selected from the list based on the assumption that they are more exposed to stressful work schedule. In the second stage, the geographical clusters of these professional groups were used. The three tertiary hospitals in Ekiti State which include Ekiti State University Teaching Hospital, Ado-Ekiti, Afe Babalola Multisystem Hospital, Ado-Ekiti and Federal Teaching Hospital, Ido-Ekiti were used in this study. The subject recruitment was done using simple random sampling of the professionals in the healthcare professional groups selected in each department of the hospitals.
2.7 Data collection procedure:
The data were collected using questionnaire and body measurements over a period of 8 weeks (July to August, 2020). The questionnaire was designed and validated for the collection of socio-demographic, work-related and lifestyle characteristics; and evaluation of perceived stress. The questionnaire was administered to the health professionals in their various units in the hospital. The body weight (in kg) was measured using a standardized bathroom weighing scale. The participants’ height was measured using a vertical height scale. The values obtained were used to calculate the Body Mass Index (BMI) by dividing the weight (kg) with the height (m2). This was categorized as underweight (BMI<18.5kg/m2), Normal (BMI=18.5-24.9kg/m2), Overweight (BMI=25.0-29.9 kg/m2) and Obese (BMI≥30.0kg/m2). The BMI measured the respondents’ nutritional status.
2.8 Perceived stress assessment:
The PSS-10 has been extensively used by researchers both globally (Alosaimi et al., 2015; Anwer et al, 2020; Huang et al.,2020; Bastianon et al., 2020) and in Nigeria (Asani et al., 2016b; Ossai et al., 2019; Ogba, 2020) for measuring perceived stress. It is a self-administered questionnaire that measures the extent to which an individual views situations as stressful and their ability to handle such stress. It is a validated measure of recent stressful experiences and it has high correlation with other measures of stressful life events like-Job Responsibilities Scale, life events scale (Cohen et al., 1983).
In this study, perceived stress of each participant was measured using this tool (Cohen et al., 1983). Each item on the questionnaire was labeled on 5-point Likert scale (Scaling: 0 = Never; 1 = Almost Never; 2 = Sometimes; 3 = Fairly often; 4 = Very often). This scale has scores between 0 and 40 based on response to specific questions. The scoring of the PSS-10 was done by summing up all the scores. The maximum obtainable score was 40. But, this was done after reversing the scores on the four positive items, e.g., 0=4, 1=3, 2=2, etc. and then summing across all the 10 items. Items 4, 5, 7, and 8 were the positively stated items, so they were reversed (Reversed Items: 4, 5, 7, 8). Thus, the Total Perceived Stress was summed as Sum Items: 1, 2, 3, 4R, 5R, 6. 7R, 8R, 9, 10. Individual scores on the PSS scale ranged between 0 and 40. Scores were classified into three, that is, 0-13 (low stress), 14-26 (moderate stress) and 27-40 (high perceived stress). For the purpose of this study, the scores ≥ 20 was considered as high level of perceived stress, that is, respondents who were considered to be stressed (Asani et al., 2016b). The Cronbach’s alpha of the PSS-10 in this study was 0.73, this indicates the reliability of the tool.
2.9 Data analysis:
Statistical Package for Social Sciences (IBM SPSS)TM version 26 was used to analyze the data. The results were presented using descriptive statistics. Chi square test was done to establish relationship between categorical variables at 5% level of significance. Variables with significant association with nutritional status were identified and a multivariate analysis was carried out to determine the predictors of nutritional status using binary logistic regression.
Results:
3.1 Socio-demographic characteristics of the healthcare professionals:
Table 1 shows the socio-demographic characteristics of the healthcare professionals. The age of the healthcare professionals ranged from 19- 65 years with a mean of 35.91±9.31 years. More than half (55.2%) were less than or equal to 35 years while about 13% were aged above 45 years. About one third (69%) of the respondents were married with a family size of 3-5 (58.3%). Running to half (45.0%) of the health professionals had practised for 6-15 years while only 6.7% of them had practiced for 26-35 years.
Table 1: Socio-demographic characteristics of the healthcare professionals| Variable | Frequency | Percent |
| Age (years) | ||
| ≤ 35 | 232 | 55.2 |
| 36 – 45 | 130 | 31.0 |
| > 45 | 58 | 13.8 |
| Mean ± SD | 35.91 ± 9.31 | |
| Range | 19 – 65 | |
| Gender | ||
| Male | 169 | 40.2 |
| Female | 251 | 59.8 |
| Religion | ||
| Christianity | 405 | 96.4 |
| Islam | 15 | 3.6 |
| Marital status | ||
| Single | 127 | 30.2 |
| Married | 290 | 69.0 |
| Divorced/ Widowed | 3 | 0.7 |
| Family size (n = 290) | ||
| < 3 | 93 | 32.1 |
| 3 – 5 | 169 | 58.3 |
| > 5 | 28 | 9.7 |
| Family type (n = 290) | ||
| Monogamous | 284 | 97.9 |
| Polygamous | 6 | 2.1 |
| Ethnicity | ||
| Yoruba | 376 | 89.5 |
| Others | 44 | 10.5 |
| Years of practice | ||
| ≤ 5 | 156 | 37.1 |
| 6 – 15 | 189 | 45.0 |
| 16 – 25 | 50 | 11.9 |
| 26 – 35 | 25 | 6.0 |
3.2 Work-related characteristics of the healthcare professionals:
The work-related characteristics of the healthcare professionals are shown in Table 2. Most (97.9%) of the respondents were interested in their job. Majority (81.7%) of the respondents reported high workload. Half (50.7%) of the healthcare professionals worked for more than 50 hours in week. Ninety-five percent of the respondents either took calls or ran shift duty at work. More than two-thirds (70.2%) of the respondents rarely experience financial difficulties while 13.8% always experience financial difficulties.
Table 2: Work-related characteristics of the healthcare professionals| Variable | Frequency | Percent |
| Interested in job | ||
| Yes | 411 | 97.9 |
| No | 9 | 2.1 |
| Self-perception of workload | ||
| Low | 50 | 11.9 |
| Moderate | 27 | 6.4 |
| High | 343 | 81.7 |
| Number of hours on duty/shift per week | ||
| 40-50 hours | 207 | 49.3 |
| 51 – 70 hours | 128 | 30.5 |
| > 70 hours | 85 | 20.2 |
| Run shifts or take calls | ||
| Yes | 399 | 95.0 |
| No | 21 | 5.0 |
| Experience financial difficulties | ||
| Never | 67 | 16.0 |
| Rarely | 295 | 70.2 |
| Always | 58 | 13.8 |
3.3 Lifestyle pattern of the healthcare professionals:
The lifestyle pattern of the healthcare professionals is revealed in Table 3. Only 10% of the healthcare professionals took alcohol and 1.9% smoke. Over 90% of the respondents engaged in physical exercise and 34.2% did that daily and 35.8% involved in it less than 3 days in a week. About 75% of the respondents slept between 6-8 hours in a day while 20.7% slept less than 6 hours daily and 91.2% took less than three meals in a day.
Table 3: Lifestyle pattern of the healthcare professionals| Variable | Frequency | Percent |
| Alcohol use | ||
| Yes | 42 | 10.0 |
| No | 378 | 90.0 |
| Cigarette smoking | ||
| Yes | 8 | 1.9 |
| No | 412 | 98.1 |
| Engage in physical exercise | ||
| Yes | 386 | 91.9 |
| No | 34 | 8.1 |
| Frequency of physical exercise/week (n = 386) | ||
| Every day | 132 | 34.2 |
| 3 – 4 days | 116 | 30.1 |
| < 3 days | 138 | 35.8 |
| Hours of sleep in a day | ||
| < 6 hours | 87 | 20.7 |
| 6 - 8 hours | 313 | 74.5 |
| > 8 hours | 20 | 4.8 |
| Number of meals/day <3 | 383 | 91.2 |
| ≥3 | 37 | 8.8 |
3.4 Perceived stress distribution of the healthcare professionals:
The distribution of the respondents based on their perceived stress is shown in Table 4. More than one third (41.9%) of the professionals sometimes were usually upset because of something that happened unexpectedly. About 37% of the respondents felt nervous and stressed sometimes; and 31.9% respondents sometimes could not cope with all they had to do. About a quarter (23.1%) of the respondents sometimes could not control irritation. More than 50% of the respondents never or almost never felt they could not overcome their difficulties, only 3.6% felt very often that difficulties were piling up and they could not overcome them.
Table 4: Perceived stress distribution of the healthcare professionals| Never | Almost never | Sometimes | Fairly often | Very Often | |
| Variable | n (%) | ||||
| Been upset because of something that happened unexpectedly | 43 (10.2) | 79 (18.8) | 176 (41.9) | 94 (22.4) | 28 (6.7) |
| Felt that you were unable to control the important things in your life | 100 (23.8) | 110 (26.2) | 128 (30.5) | 55 (13.1) | 27 (6.4) |
| Felt nervous and “stressed” | 37 (8.8) | 73 (17.4) | 156 (37.1) | 90 (21.4) | 64 (15.2) |
| Felt confident about your ability to handle your personal problems | 12 (2.9) | 27 (6.4) | 64 (15.2) | 126 (30.0) | 191 (45.5) |
| Felt that things were going your way | 14 (3.3) | 33 (7.9) | 117 (27.9) | 156 (37.1) | 100 (23.8) |
| Found that you could not cope with all the things that you had to do | 84 (20.0) | 116 (27.6) | 134 (31.9) | 63 (15.0) | 23 (5.5) |
| Been able to control irritations in your life | 14 (3.3) | 36 (8.6) | 97 (23.1) | 156 (37.1) | 117 (27.9) |
| Felt that you were on top of things | 25 (6.0) | 38 (9.0) | 109 (26.0) | 156 (37.1) | 92 (21.9) |
| Been angered because of things that were outside of your control | 59 (14.0) | 122 (29.0) | 144 (34.3) | 70 (16.7) | 25 (6.0) |
| Felt difficulties were piling up so high that you could not overcome them | 127 (30.2) | 137 (32.6) | 101 (24.0) | 40 (9.5) | 15 (3.6) |
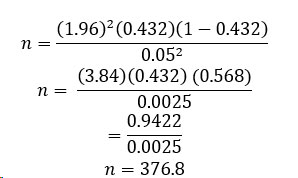
3.5 Prevalence of perceived stress among healthcare professionals:
The mean PSS score was 15.02 ± 6.16. The prevalence of perceived stress among the healthcare professionals is depicted in figure 2. The prevalence of perceived stress was found to be 47.6%.
3.6 Nutritional status of the healthcare professionals:
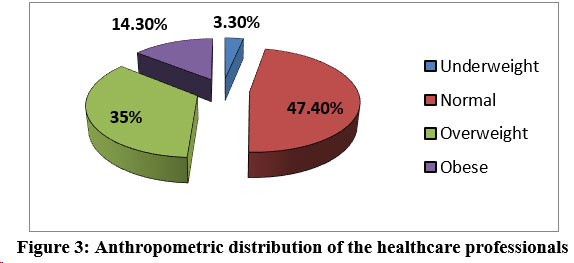
Figure 3 shows the anthropometric distribution of the healthcare professionals with 3.3% underweight, 35.0% overweight and 14.3% obese.
3.7 Association between socio-demographic characteristics and perceived stress of the healthcare professionals:
Table 5 below shows the association between socio-demographic characteristics and perceived stress of the healthcare professional. There was significant association (p=0.016) between the age of the respondents and their perceived stress with stress increasing as the age decreasing. There was also significant association between the gender of the respondents and their perceived stress (p=0.001). More (54.2%) female respondents reported being stressed than their male counterparts (37.9%). Marital status also showed significant statistical association with perceived stress (p=0.001), about 60% of those who were single reported being stressed compared to 42.1% of those who were married. The different professional groups had statistically significant association with perceived stress (p=0.048). More than half of the nurses and almost half of the doctors reported being stressed while less than 30% of Medical laboratory scientists reported being stressed.
Table 5: Association between socio-demographic characteristics and perceived stress of the healthcare professionals
| Perceived stress | |||||
| Variable | Stressed | Not stressed | Total | χ2 | p-value |
| n (%) | n (%) | N (%) | |||
| Age (years) | |||||
| ≤ 35 | 125 (53.9) | 107 (46.1) | 232 | 8.218 | 0.016* |
| 36 – 45 | 51 (39.2) | 79 (60.8) | 130 | ||
| >45 | 24 (41.4) | 34 (58.6) | 58 | ||
| Sex | |||||
| Male | 64 (37.9) | 105 (62.1) | 169 | 10.776 | 0.001* |
| Female | 136 (54.2) | 115 (45.8) | 251 | ||
| Marital status | |||||
| Single | 77 (60.6) | 50 (39.4) | 127 | 12.510F | 0.001* |
| Married | 122 (42.1) | 168 (57.9) | 290 | ||
| Divorced/ Widowed | 1 (33.3) | 2 (66.7) | 3 | ||
| Family size (n = 290) | |||||
| < 3 | 43 (46.2) | 50 (53.8) | 93 | 4.030 | 0.133 |
| 3 – 5 | 72 (42.6) | 97 (57.4) | 169 | ||
| > 5 | 7 (25.0) | 21 (75.0) | 28 | ||
| Family type (n = 290) | |||||
| Monogamous | 120 (42.3) | 164 (57.7) | 284 | 0.192F | 1.000 |
| Polygamous | 2 (33.3) | 4 (66.7) | 6 | ||
| Years of practice | |||||
| ≤ 5 | 85 (54.5) | 71 (45.5) | 156 | 5.226 | 0.156 |
| 6 – 15 | 85 (45.0) | 104 (55.0) | 189 | ||
| 16 – 25 | 20 (40.0) | 30 (60.0) | 50 | ||
| 26 – 35 | 10 (40.0) | 15 (60.0) | 25 | ||
| Profession | |||||
| Doctor | 75 (46.0) | 88 (54.0) | 163 | 6.083 | 0.048* |
| Nurse | 115 (51.6) | 108 (48.4) | 223 | ||
| Medical laboratory scientist | 10 (29.4) | 24 (70.6) | 34 | ||
3.8 Association between perceived stress and nutritional components:
There was no statistically significant association between the perceived stress and nutritional components of the respondents as shown in table 6.
Table 6: Association between perceived stress and nutritional components| Perceived stress | |||||
| Stressed | Not stressed | Total | χ2 | p value | |
| Variable | n (%) | n (%) | N | ||
| Body Mass Index | |||||
| Underweight | 7(50.0) | 7(50.0) | 14 | 0.562 | 0.905 |
| Normal | 91(45.7) | 108(54.3) | 199 | ||
| Overweight | 72(49.0) | 75(51.0) | 147 | ||
| Obese | 30(50.0) | 30(50.0) | 60 | ||
3.9 Predictors of stress among the healthcare professionals:
As shown in Table 7, the statistically significant independent predictors of stress among the healthcare professionals were gender and marital status. Male healthcare professionals had lesser odds of being stressed as compared with the female ones (OR: 0.512; p value 0.008). Furthermore, those who were single had about 2 times increase in the odds of being stressed as compared with the married healthcare professionals (OR: 1.762; p value 0.040).
Table 7: Predictors of stress among the healthcare professionals| Variable | B | OR (95% CI) | p value |
| Age (years) | |||
| ≤ 35 | 0.219 | 1.245 (0.640 – 2.421) | 0.519 |
| 36 – 45 | -0.002 | 0.998 (0.518 – 1.920) | 0.994 |
| > 45 REF | 1 | ||
| Gender | |||
| Male | -0.683 | 0.505 (0.308 – 0.830) | 0.007* |
| Female REF | 1 | ||
| Marital status | |||
| Married REF | 1 | ||
| Single | 0.649 | 1.914 (1.143 – 3.208) | 0.014* |
| Divorced/ Widowed | -0.590 | 0.554 (0.048 – 6.342) | 0.635 |
| Profession | |||
| Doctor REF | 1 | ||
| Nurse | -0.022 | 0.979 (0.586 – 1.634) | 0.934 |
| Medical laboratory scientist | -0.088 | 0.599 (0.262 – 1.369) | 0.224 |
Discussion:
4.1 Socio-demographic characteristics of respondents
This category of healthcare professionals constitutes a dominant workforce and the major drivers of productivity in the health sector, so the issue of their nutrition in relation to stress is a crucial matter. Majority of the healthcare professionals that participated in the study had many years of job experience and would have been better able to manage stress on the job. About half of the respondents were young and middle aged adults with a small family size.
4.2 Nutritional status of respondents
Anthropometric indicators were used to measure nutritional status. Half of the respondents were overweight and obese. This confirms the recent meta-analysis which estimated high prevalence of overweight and obesity in Nigeria (Adeloye et al., 2021); it is lower to 70% reported by Adeomi et al. (2020) and higher than 24.0% among the market women (Dada, 2017) and 47% among the healthcare workers (Banwat et al., 2018) in Nigeria. The possible reason for this finding could be sedentary lifestyle and high prevalence of work-related stress. Majority of the respondents carried high workload at work and only one third carried out physical body exercise daily. These two factors have been reported as risk factors of obesity (Olaitan et al., 2020). It has been reported that obesity can cause absenteeism and lower employee’s productivity and efficiency (Olaitan et al., 2020). It follows, therefore, normal body weight enhances workers’ agility, work productivity and reduced tendency to develop obesity-related disease such as hypertension, diabetes, and osteoarthritis. However, excessive accumulation of weight may weaken their agility and adversely affect patient care which demands increased nurse-patient interaction. This high prevalence of overweight and obesity among the healthcare professionals puts the entire population in a greater risk since the healthcare professionals are the major care taker of the overall community health issues.
4.3 Perceived stress of the respondents
This study also revealed a high level of perceived stress with about half of the respondents being stressed, which was higher compare to 32% and 43% obtained among medical doctors in Ibadan (Adeolu et al., 2016) and in Ile-Ife (Akinsulore et al., 2020), Nigeria respectively. This finding was lower in comparison with studies done in Portugal (50%) (Joaquim et al., 2017), Iran (78.4%), Saudi Arabia (66.2%) and United Kingdom (59%) (Kakemam et al., 2019; Isfahani et al., 2020). The outcomes of studies from different countries revealed variations in the prevalence of perceived stress among health care professionals. This might be due to reasons which include differences in sample size, study population, socioeconomic level and measurement tool. For example, the studies carried out in Iran involved only nurses and different scales like nursing stress scales were used to evaluate stress.
There was significant association between the age, gender, marital status and profession of the respondents and perceived stress. Female and single healthcare professionals had higher odds of being stressed as compared with the male and married ones. This implies that these two factors were predictors of being stressed among the respondents. This finding of female respondents being more stressed than their male counterparts was similar to some previous studies (Haile, 2017; Godifay et al., 2018; Worku et al., 2020). The multiple responsibilities of females outside their work place could be responsible for this. However, study done by Adeolu et al. (2016) showed no gender association with perceived stress. Similarly, single healthcare professionals were more stressed as compared to married ones, this was also found in some previous studies (Godifay et al., 2018; Nemera 2018; Worku et al., 2020). This could be attributed to their lack of experience, lack of family support and life challenges characteristics of young adult life. The medical laboratory scientists were the least stressed followed by doctors and nurses. The nurses are traditionally more in contact with patients than other healthcare professionals. This might explain their higher level of stress than others. Adeolu et al. (2016) reported no significant associations between job stress and socio-demographic characteristics. Stress may prevent or reduce people’s involvement in physical activity which has been found to be associated with prevalence of overweight and obesity. However, in this current study the Body Mass Index of the participants was not found to be significantly related to the perceived stress.
Conclusion:
In this study, we focused on perceived stress and the nutritional status of health care professionals. The finding of this study showed that about half of the healthcare professionals experienced work-related stress and notably in females, singles, young adult and nursing professionals with the independent predictors of stress among the healthcare professionals being gender and marital status.
Recommendations:
Appropriate policy targeted on reducing the healthcare professionals’ workload and incorporating recreational programme to their daily routine should be put in place by Government and other stakeholders in healthcare in Nigeria. In addition, nutrition education is recommended to be included in the scheme of on-the-job training of healthcare professionals. Further research that will involve a more comprehensive assessment of stress and its impact on the different nutritional indicators is also advised.